The intersection of acute-onset psychiatric symptoms and neurological decline in young patients presents a critical diagnostic challenge. Prompt identification is vital for prognosis.
Let’s review a classic clinical presentation and a highly specific neurophysiological biomarker that every neurologist, psychiatrist, and critical care specialist should recognize.
The Clinical Picture
A 17-year-old female is brought to the emergency department with a subacute onset of severe behavioral changes over the past week. Her history is notable for insomnia, agitation, and grandiose delusions (believing she is a famous spy).
Physical examination reveals new-onset orofacial dyskinesias (unusual movements of the lips and mouth). During triage, she suffers a generalized tonic-clonic seizure and subsequently rapidly progresses to severe encephalopathy, requiring critical care admission.
This constellation of symptoms—psychosis, movement disorders, seizures, and autonomic instability—in a young female is highly suggestive of an autoimmune etiology.
The Neurophysiological Clue: “Extreme Delta Brush”
While seizures are a core component of this syndrome, initial EEGs are frequently non-specific, often showing only diffuse slowing or disorganized activity.
However, approximately 25% of these patients exhibit a pathognomonic EEG pattern that can significantly accelerate diagnosis: the Extreme Delta Brush.
Defining the Pattern:
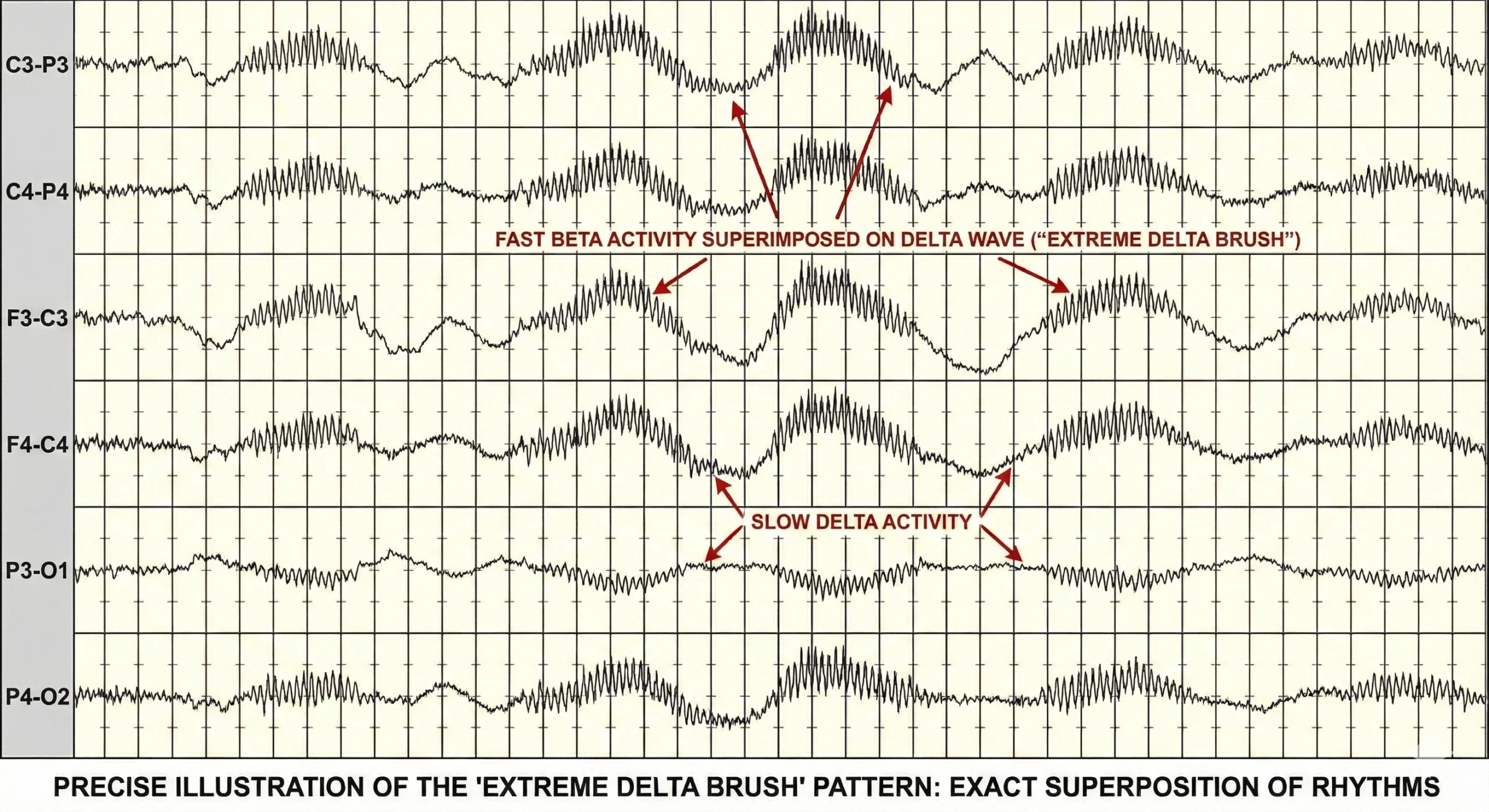
As illustrated above, the “Extreme Delta Brush” is characterized by a unique superposition of rhythms:
The Foundation: Rhythmic, high-amplitude delta (δ) activity typically in the 1–3 Hz range.
The “Brush”: Superimposed bursts of rhythmic, fast beta (β) frequency activity (20–30 Hz) literally “riding” the crests and troughs of the slow delta waves.
It is this exact grafting of fast activity onto slow waves that gives the waveform its characteristic serrated or “brushed” appearance.
The Diagnosis: Anti-NMDA Receptor Encephalitis
This clinical presentation combined with the “extreme delta brush” pattern strongly points to Anti-NMDAR (N-methyl-D-aspartate receptor) Encephalitis.
Pathophysiology: An autoimmune disorder mediated by IgG antibodies against the GluN1 subunit of the NMDA receptor.
Associations: It is frequently a paraneoplastic phenomenon, most commonly associated with ovarian teratomas in young female patients.
Confirmation: Definitive diagnosis requires the detection of IgG GluN1 antibodies in cerebrospinal fluid (CSF) and/or serum.
Differential Considerations
While Anti-NMDAR is the most probable diagnosis in this specific scenario, the differential for autoimmune encephalopathy is broad and includes entities mediated by antibodies against:
LGI1 & CASPR2: Often presenting with limbic encephalitis, neuromyotonia, or insomnia (CASPR2 is often associated with thymoma).
AMPA & GABA-A receptors: Frequently presenting with acute seizures or refractory status epilepticus, also with high rates of underlying malignancies.
Management Principles
Time is brain in autoimmune encephalitis. Outcomes are directly linked to the rapidity of treatment initiation.
First Line: Aggressive immunotherapy with high-dose steroids and IVIG or plasmapheresis.
Second Line: Many patients with significant symptomatology will require escalation to second-line agents like rituximab or cyclophosphamide.
Concurrent Workup: A thorough screening for an underlying malignancy (chest/abdomen/pelvis CT, pelvic ultrasound/MRI) is mandatory.
Key Takeaways for the Clinician
Maintain a high index of suspicion for autoimmune encephalitis in young patients presenting with acute “psychiatric” breaks accompanied by neurological soft signs (movement disorders, seizures).
Scrutinize the EEG for the “Extreme Delta Brush”—rhythmic delta waves carrying superimposed fast beta bursts. Its presence is a powerful diagnostic accelerator.
Do not wait for antibody confirmation to initiate empirical immunotherapy if the clinical suspicion is high (Probable diagnostic criteria are met).
Have you encountered this pattern in your practice? Share your experiences below.

Pingback: Neurology Board Review: 10 High-Yield Epilepsy Questions Explained - NeuromedHub