In clinical neurology, the history tells you what the pathology is, but the examination tells you where the lesion is. For medical students and residents preparing for exams (like the MRCP, Prometric or Boards), mastering stroke localization is not just about memorizing the Circle of Willis, it is about understanding the functional geography of the brain.
This guide provides a comprehensive breakdown of the major vascular territories, their sub-divisions, and the classic clinical syndromes associated with their occlusion.
1. The Anterior Circulation
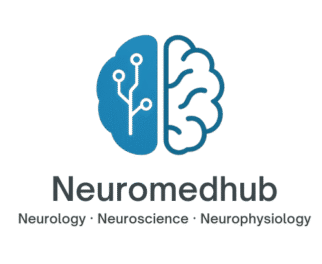
The anterior circulation is supplied by the Internal Carotid Arteries (ICA) and accounts for roughly 80% of the blood supply to the brain.
A. Middle Cerebral Artery (MCA) The MCA is the most common site of ischemic stroke. It supplies the lateral surface of the frontal, temporal, and parietal lobes. However, for exam purposes, you must distinguish between the main stem and its divisions.
MCA Main Stem (M1) Occlusion:
Contralateral Hemiplegia & Hemianesthesia: Affecting the face and arm > leg.
Global Aphasia (Left/Dominant): Total loss of expressive and receptive language.
Gaze Deviation: Eyes look toward the lesion.
Superior Division (Anterior branches):
Supplies the frontal lobe.
Deficit: Dense motor weakness (face/arm) and Broca’s Aphasia (expressive non-fluent aphasia) if in the dominant hemisphere.
Key feature: Sensory function is often spared.
Inferior Division (Posterior branches):
Supplies the temporal/parietal lobes.
Deficit: Wernicke’s Aphasia (receptive fluent aphasia) if in the dominant hemisphere.
Visual Deficit: Contralateral superior quadrantanopia (“Pie in the sky”).
Key feature: Motor function is often spared, but the patient may seem confused or “psychotic” due to language comprehension loss.
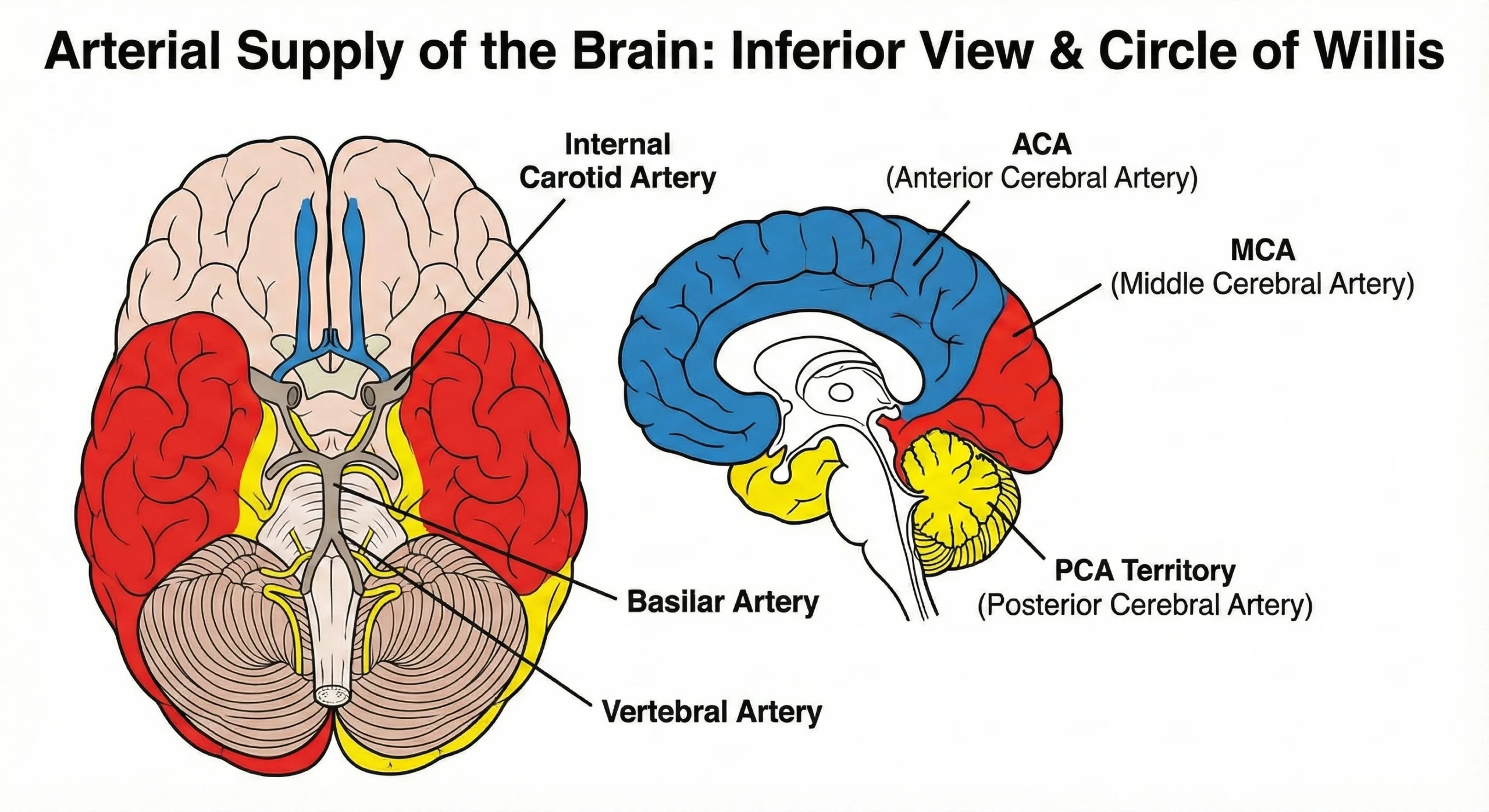
B. Anterior Cerebral Artery (ACA)
The ACA supplies the medial surface of the frontal and parietal lobes.3 This area corresponds to the “leg and foot” area of the motor homunculus.
Key Clinical Features:
Contralateral hemiparesis and sensory loss: Prominently affecting the leg and foot > arm/face.
Frontal Release Signs: Grasp reflex, sucking reflex, snout reflex.
Behavioral Changes: Abulia (lack of initiative), urinary incontinence (paracentral lobule involvement), and akinetic mutism in bilateral damage.
Transcortical Motor Aphasia: Similar to Broca’s but with preserved repetition.4
2. The Posterior Circulation
Supplied by the Vertebral and Basilar arteries, this system perfuses the brainstem, cerebellum, and occipital lobes.
A. Posterior Cerebral Artery (PCA)
The PCA supplies the occipital cortex (vision), the inferomedial temporal lobe, and the thalamus.5
Key Clinical Features:
Contralateral Homonymous Hemianopsia: Visual field loss on the opposite side, often with “macular sparing” (due to dual supply from the MCA at the occipital pole).
Alexia without Agraphia: A classic board question. Occurs with a Left PCA infarct involving the splenium of the corpus callosum. The patient can write but cannot read what they just wrote.
Thalamic Syndrome (Dejerine-Roussy): Severe, intractable, burning pain on the contralateral side of the body.
B. The “Top of the Basilar” Syndrome
Embolic occlusion at the top of the basilar artery can cause ischemia to the midbrain and thalamus bilaterally.6
Signs: Reduced consciousness, oculomotor issues (vertical gaze palsy), and hallucinations (peduncular hallucinosis).
3. Brainstem Syndromes (The “Crossed” Signs)
The hallmark of a brainstem lesion is “crossed findings”: cranial nerve deficits on the ipsilateral (same) side and long-tract motor/sensory deficits on the contralateral (opposite) side.7
A. Lateral Medullary (Wallenberg) Syndrome
Vessel: PICA (Posterior Inferior Cerebellar Artery) or Vertebral Artery.
Ipsilateral Signs: Facial numbness (CN V nucleus), Horner’s syndrome (sympathetics), Ataxia (inferior cerebellar peduncle), Dysphagia/Hoarseness (Nucleus Ambiguus – CN IX, X).
Contralateral Signs: Loss of pain/temperature in the body (Spinothalamic tract).
Note: No motor weakness in the limbs (pyramids are medial).
B. Medial Medullary Syndrome
Vessel: Anterior Spinal Artery.
Ipsilateral Signs: Tongue deviation (CN XII).
Contralateral Signs: Hemiparesis (Pyramids) and loss of vibration/proprioception (Medial Lemniscus).8
C. Weber’s Syndrome (Midbrain)
Vessel: PCA perforators.
Ipsilateral Signs: CN III palsy (down and out eye, dilated pupil, ptosis).
Contralateral Signs: Hemiparesis.
4. Lacunar Syndromes (Small Vessel Disease)
These are small infarcts (0.2–15 mm) in the deep cerebral white matter, basal ganglia, or pons, usually due to lipohyalinosis from chronic hypertension. They lack “cortical” signs (no aphasia, no neglect, no visual field loss).
Pure Motor Stroke: Injury to the Posterior Limb of the Internal Capsule.10 (Most common).
Pure Sensory Stroke: Injury to the VPL nucleus of the Thalamus.
Ataxic Hemiparesis: Injury to the Pons or Internal Capsule.11
Dysarthria-Clumsy Hand Syndrome: Injury to the Pons or Genu of the Internal Capsule.
5. Watershed Infarcts
These occur at the border zones between major vascular territories, usually due to systemic hypoperfusion (e.g., cardiac arrest or severe hypotension) rather than embolism.
ACA-MCA Watershed: Leads to “Man-in-the-Barrel” syndrome. The patient has proximal weakness of the shoulders and hips (trunk) with sparing of the face, hands, and feet.
MCA-PCA Watershed: Can cause disturbances in higher-order visual processing (Balint syndrome).
Summary Table for Quick Revision
| Artery | Primary Deficit | Key Localization Clue |
| MCA | Face/Arm Weakness | Aphasia (Left) or Neglect (Right) |
| ACA | Leg/Foot Weakness | Urinary Incontinence, Personality Change |
| PCA | Visual Field Cut | Macular Sparing, Alexia w/o Agraphia |
| PICA | Vertigo, Ataxia | Crossed Sensory Loss, Horner’s Syndrome |
| Lacunar | Pure Motor/Sensory | NO Aphasia, NO Visual Cut |