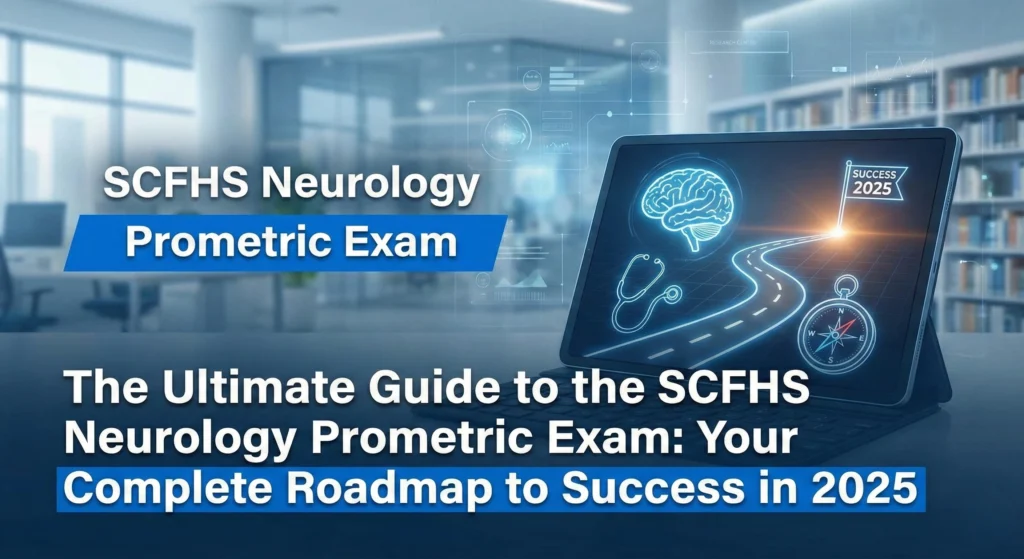
When you’re preparing for the SCFHS Neurology Prometric exam, you’re not just studying for any licensing test—you’re working toward a credential that unlocks your career across the entire Gulf region. Yet despite its critical importance, finding a comprehensive, trustworthy guide specifically tailored to this exam has been nearly impossible. Most resources online are either outdated, overly generic, or focus on selling MCQ banks rather than actually helping you understand what you’re up against.
This guide is different. It’s built on official SCFHS blueprints, real exam structures, and the proven strategies that work for neurologists and clinical neurophysiologists seeking specialist or consultant classification in Saudi Arabia and beyond.
Understanding the SCFHS Neurology Prometric Exam
The SCFHS (Saudi Commission for Health Specialties) Neurology Prometric exam is the standardized licensing assessment required for medical professionals seeking professional classification and practice rights across Saudi Arabia and multiple GCC countries. While other Gulf nations like the UAE (DHA), Oman (DOH), and Qatar (QCHP) have similar examinations, the SCFHS framework represents the most comprehensive and widely recognized licensing standard in the region.
Who Absolutely Needs This Exam?
Neurology Specialists and Residents
If you’ve completed your neurology training and want to practice in Saudi Arabia, this exam is non-negotiable. It’s the official assessment tool used by SCFHS to verify that your clinical knowledge meets Saudi healthcare standards.
Clinical Neurophysiologists (EEG/EMG Specialists)
Even though clinical neurophysiology is sometimes recognized as a separate specialty in some countries, SCFHS classifies it under neurology. If you specialize in electromyography, nerve conduction studies, or electroencephalography, you’ll be taking the same neurology exam. There’s no separate pathway for clinical neurophysiologists—it’s all neurology from SCFHS’s perspective.
International Medical Graduates (IMGs)
Neurologists trained outside the Kingdom face additional scrutiny and must prove their competence through this examination. The exam is particularly critical if you’ve trained in countries like India, Pakistan, Egypt, the United Kingdom, or the United States, as it’s SCFHS’s way of ensuring equivalency in knowledge and clinical reasoning.
Physicians Seeking Career Advancement
Many hospitals in Saudi Arabia won’t finalize your employment contract or promote you to specialist or consultant status without a passing score. This exam often becomes a mandatory professional milestone before you can take on leadership roles or higher-paying positions.
The Official Exam Structure: What You Need to Know
SCFHS has been transparent about the exam format, and understanding it exactly is your first competitive advantage.
Exam Format and Content
Format: Computer-Based Test (CBT) administered through Prometric centers worldwide
Duration: 4 hours (240 minutes) with no break built in
Number of Questions: 200 Multiple-Choice Questions (MCQs), single-best-answer format
Question Types: All questions follow the K1, K2, and K3 difficulty levels:
K1 (Knowledge): Pure recall of facts and definitions
K2 (Comprehension): Understanding and interpreting clinical information
K3 (Application): Applying knowledge to real clinical scenarios and decision-making
Delivery: Online proctored or in-person at authorized Prometric test centers
Passing Scores (The Official Numbers)
Registrar/Specialist Level: 65%
Senior Registrar: 70%
Important: These scores can be adjusted slightly by SCFHS depending on the statistical performance of the entire cohort. If fewer than 70% of candidates pass, the score may be lowered incrementally, but it will never go below 60%. This is helpful to know—a difficult year may work in your favor.
The Official SCFHS Neurology Blueprint (2024-2025)
This is the exact content distribution directly from SCFHS. Knowing these percentages should completely shape your study strategy.
| Domain | Percentage | Question Count (Approx.) |
|---|---|---|
| Cerebrovascular Disorders | 15% | 30 |
| Epilepsy and Paroxysmal Disorders | 15% | 30 |
| Cephalgia and Headache Disorders | 15% | 30 |
| Cognitive Disorders | 7% | 14 |
| Movement Disorders | 7% | 14 |
| Neuro-Immunological Disorders | 7% | 14 |
| Neuro-Infectious Disorders | 7% | 14 |
| Neuromuscular Disorders | 7% | 14 |
| Neurology of Systemic Diseases | 5% | 10 |
| Clinical Neurophysiology (EEG/EMG) | 5% | 10 |
| Patient Safety and Quality Improvement | 5% | 10 |
| Professionalism and Ethics | 5% | 10 |
| TOTAL | 100% | 200 |
Note: Blueprint distributions may vary by ±5% in each category. Always check the official SCFHS website for the most current version.
This blueprint is your bible. Everything you study should tie back to this distribution. If cerebrovascular disorders are 15% of the exam, they deserve 15% of your study time—not less.
High-Yield Topics: Where Your Study Time Matters Most
The following topics appear repeatedly on the exam and often determine who passes and who doesn’t. These are the areas where a single missed question can cost you.
1. Cerebrovascular Disorders (15% – Your Highest Yield Topic)
Stroke is the most heavily weighted domain. Expect multiple questions on acute management, prevention, and long-term care.
Must-Know Sub-topics:
IV Thrombolysis (rtPA/Alteplase): Inclusion/exclusion criteria, contraindications, time windows (3-4.5 hours), BP management before and after thrombolysis, monitoring for complications
Mechanical Thrombectomy: Indications, patient selection, time window, large vessel occlusion (LVO) criteria
Blood Pressure Management: Target BP pre-thrombolysis (< 185/110), post-thrombolysis management, when to lower BP and when not to
Anticoagulation: Indications for anticoagulation, drug selection (warfarin vs. DOACs), contraindications, HAS-BLED scores
Antiplatelet Therapy: When to start aspirin, clopidogrel resistance, dual antiplatelet therapy in acute stroke
Stroke Mimics: Conditions that look like stroke but aren’t (hypoglycemia, seizures, migraine, Todd’s paralysis, functional disorders)
Secondary Stroke Prevention: Statin therapy, blood pressure targets, lifestyle modifications, risk factor management
Hemorrhagic Transformation: Timing, risk factors, clinical significance
Posterior Circulation Stroke: Vertebrobasilar artery occlusion, specific management considerations
2. Epilepsy and Paroxysmal Disorders (15% – Second Highest)
This is equally weighted with stroke and demands equal preparation.
Must-Know Sub-topics:
Status Epilepticus (SE): Definition (seizure lasting > 5 minutes), first-line treatment (benzodiazepines—lorazepam, midazolam), second-line agents (phenytoin, fosphenytoin, levetiracetam, valproate), third-line options (propofol, midazolam infusion)
Seizure Classification: Generalized vs. focal seizures, tonic-clonic vs. absence vs. myoclonic, current ILAE classification
EEG Patterns: 3-Hz spike-and-wave (absence seizures), focal spikes, polyspike-and-wave, generalized paroxysmal fast activity
Antiepileptic Drugs (AEDs): First-line agents (valproate, levetiracetam, lamotrigine), second-line agents, teratogenicity concerns, drug interactions
Special Populations: Pregnancy and AEDs, elderly patients, drug-drug interactions
Provoked vs. Unprovoked Seizures: When to start long-term AED therapy
Neonatal Seizures: Causes, phenobarbital use, timing of investigations
3. Cephalgia and Headache Disorders (15% – Equally Critical)
Headache is a common chief complaint, and SCFHS expects you to differentiate types and manage appropriately.
Must-Know Sub-topics:
Red Flags in Headache: Thunderclap headaches, fever + meningismus, focal neurologic deficits, sudden onset in elderly, progressive nature, change in pattern
Migraine: Diagnostic criteria, prodrome/aura, management (triptans, NSAIDs, antiemetics), preventive therapy (propranolol, amitriptyline, topiramate, CGRP inhibitors)
Tension-Type Headache: Diagnostic features, management
Cluster Headache: Clinical presentation, acute and preventive treatment (oxygen, triptans, verapamil)
Idiopathic Intracranial Hypertension (IIH): Risk factors (obese females), papilledema, visual threats, LP findings, management
Meningitis: Bacterial vs. viral, CSF findings, empiric antibiotic therapy timing
Subarachnoid Hemorrhage (SAH): Classic thunderclap presentation, CT findings, LP (xanthochromia), ruptured aneurysm management, vasospasm prevention
Medication Overuse Headache: When analgesics become the problem
Secondary Headaches: Temporal arteritis (giant cell arteritis), hypertensive emergency, sinusitis
4. Neuromuscular Disorders (7% – High-Yield Details)
Clinical neurophysiology candidates should study this extensively.
Must-Know Sub-topics:
Myasthenia Gravis (MG): Antibody testing (anti-acetylcholine receptor), repetitive nerve stimulation (>10% decrement = post-synaptic), single-fiber EMG, edrophonium test, management (anticholinesterase, immunosuppression)
Guillain-Barré Syndrome (GBS): Ascending paralysis, autonomic instability, CSF findings (albuminocytologic dissociation), EMG patterns, management (IVIG, plasmapheresis)
CIDP (Chronic Inflammatory Demyelinating Polyneuropathy): Demyelination on EMG, progressive nature, treatment escalation
ALS (Amyotrophic Lateral Sclerosis): UMN + LMN signs, fasciculations, El Escorial criteria, bulbar involvement, respiratory compromise
Muscular Dystrophies: Duchenne vs. Becker, dystrophin, elevated CPK, muscle biopsy findings
Neuropathies: Diabetic (distal sensorimotor), inflammatory, toxic (alcohol, chemotherapy), nutritional, NCS/EMG patterns
5. Movement Disorders (7%)
Must-Know Sub-topics:
Parkinson’s Disease: Cardinal features (bradykinesia, rigidity, resting tremor, postural instability), dopamine agonists, L-DOPA, motor fluctuations, on-off phenomenon
Wilson Disease: Ceruloplasmin, slit-lamp examination (Kayser-Fleischer rings), MRI findings, chelation therapy
Essential Tremor vs. Parkinson’s Tremor: Distinguishing features, management
Dystonia: Task-specific vs. generalized, treatment with botulinum toxin
Tremor Differential: Resting, postural, kinetic, orthostatic
6. Neuro-Immunological Disorders (7%)
Must-Know Sub-topics:
Multiple Sclerosis (MS): McDonald Criteria for diagnosis, demyelinating plaques on MRI, oligoclonal bands in CSF, MS subtypes (RRMS, PPMS, SPMS), disease-modifying therapies, relapse management with high-dose IV methylprednisolone
Transverse Myelitis (TM): Complete or incomplete myelitis, CSF findings, MRI cord lesions
ADEM (Acute Disseminated Encephalomyelitis): Monophasic vs. MS, multifocal white matter lesions, CSF findings
NMO Spectrum Disorder (NMOSD): Aquaporin-4 antibodies, optic neuritis + myelitis, management differences from MS
7. Neuro-Infectious Disorders (7%)
Must-Know Sub-topics:
Bacterial Meningitis: Classic CSF findings (elevated WBC with PMN predominance, elevated protein, low glucose), empiric antibiotics (ceftriaxone, vancomycin), dexamethasone timing
Viral Meningitis/Encephalitis: HSV encephalitis (temporal lobe involvement on MRI), acyclovir therapy, CSF findings (lymphocytic predominance, normal glucose)
TB Meningitis: Subacute presentation, very high protein in CSF, low glucose, acid-fast bacilli, isoniazid + rifampicin + pyrazinamide + ethambutol
Fungal Meningitis: CSF India ink, cryptococcal antigen testing, amphotericin B
Neurosyphilis: Neurosyphilis serology, CSF VDRL, penicillin treatment
HIV-Related Neurologic Complications: CD4 count thresholds for opportunistic infections (CMV at CD4 < 50), PML, cryptococcosis
8. Clinical Neurophysiology (EEG/EMG – 5%)
Critical for clinical neurophysiologist candidates.
Must-Know Sub-topics:
EEG Interpretation: Normal rhythms (alpha, beta, theta, delta), abnormal patterns (spike-and-wave, focal slowing), burst suppression
EMG Basics: Motor units, recruitment patterns, interference patterns, fibrillations, fasciculations, motor unit action potentials (MUAPs)
NCS (Nerve Conduction Studies): Demyelination vs. axonal patterns, conduction blocks, slowed velocities
Repetitive Nerve Stimulation: Neuromuscular junction disorders
Single-Fiber EMG: Increased “jitter” in myasthenia gravis
9. Patient Safety and Professionalism (10% Combined – Don’t Overlook)
This often determines the difference between a pass and a fail because candidates underestimate it.
Must-Know Sub-topics:
Medication Safety: Correct dosing, avoiding drug interactions, checking for allergies
Infection Control: Hand hygiene, sterile procedures, isolation precautions
Informed Consent: Ethical principles, shared decision-making
Confidentiality and Data Privacy: Patient information protection
Falls Prevention: Especially in elderly patients
Diagnostic Errors: Common pitfalls in neurology (stroke mimics, misdiagnosed seizures)
The Official Registration and Exam Booking Process
Navigating the SCFHS bureaucracy can be frustrating, but understanding each step will prevent months of delays.
Step 1: Initial Application Through Mumaris Plus
Access the SCFHS online portal at Mumaris Plus (mumaris.scfhs.org.sa). Create your account and select “Professional Classification” for specialist or consultant-level applicants.
Required Documents:
Original MBBS or equivalent medical degree certificate
Residency/specialization completion certificate
Internship (house job) certificate
Training logbook (if applicable)
Experience certificates from previous employers
Valid passport with bio page
Recent passport-style photograph (white background)
Professional license from your home country
Ensure every single detail on these documents matches perfectly. Discrepancies in name spellings, dates, or credentials are the #1 cause of application rejection.
Step 2: SCFHS Document Review and Classification
SCFHS staff review your submitted documents to verify that your qualifications meet their Professional Qualification Requirements (PQR). If approved, they officially “classify” you, recognizing your specialist designation.
This step typically takes 2-4 weeks but can extend longer if documents are incomplete.
Step 3: The DataFlow Primary Source Verification (PSV)
This is mandatory and non-negotiable. SCFHS will automatically initiate a case with DataFlow Group, an independent credential verification company. DataFlow contacts your:
Universities (degree verification)
Previous employers (experience verification)
Professional licensing boards (licensure verification)
This verification period takes 3-8 weeks, depending on how quickly your institutions respond. International universities and licensing bodies often move slowly, so factor in extra time if you trained abroad.
You cannot proceed to book the exam without a completed and “Positive” DataFlow report.
Step 4: Receive Your Eligibility Number
Once DataFlow confirms everything and SCFHS approves your application, you’ll receive an Eligibility Number in your Mumaris Plus dashboard. This is your golden ticket.
Step 5: Book Your Prometric Exam
Visit the official Prometric website (prometric.com), enter your eligibility number, and select:
SCFHS as the testing authority
Your preferred test center (Prometric has centers in most countries)
Your desired exam date
Exam Fees:
SCFHS Classification fee: ~SAR 200
DataFlow PSV fee: SAR 400-900 (varies by document count)
Prometric exam fee: ~$220-250 USD
Total Expected Cost: $400-600 USD
Step 6: Take the Exam
Arrive 30 minutes early. Bring:
Valid passport (required for identification)
Exam confirmation letter (from Prometric)
Any other documents requested in your appointment confirmation
The exam is administered at a computer terminal with strict proctoring. You cannot bring notes, calculators, or unauthorized materials.
Step 7: Results
SCFHS typically releases results within 7-14 days. Your Mumaris Plus dashboard will automatically update with your pass/fail status.
Official SCFHS Study Resources and References
SCFHS officially recommends these textbooks. While they don’t endorse any single resource exclusively, these are the gold standard:
Core Neurology Textbooks
Bradley’s Neurology in Clinical Practice – Comprehensive, modern, excellent for clinical correlation
Principles of Neurology (Adams & Victor) – Classic reference, detailed pathophysiology
Merritt’s Neurology – Practical, clinically oriented, easier to read than Adams
Localization in Clinical Neurology (Brazis, Masdeu, Biller) – Essential for understanding where lesions are
Neurological Differential Diagnosis (John Patten) – Perfect for MCQ preparation
Ethics and Professionalism
Professionalism and Ethics Handbook for Residents – SCFHS official resource
Essentials of Patient Safety – SCFHS official resource
These SCFHS-published ethics and safety documents are often the source of 5-10% of exam questions. Download them directly from SCFHS.

High-Yield Resources for MCQ Practice
Since this is an MCQ exam, you need high-quality question banks. While SCFHS doesn’t officially publish practice questions, Several online platforms offer neurology MCQs, but many of these question banks suffer from poor accuracy and frequent errors. Here, we aim to provide high-quality practice questions that mirror more than 95% of the style, difficulty, and format of the real Prometric Neurology exam—complete with clear explanations and updated references.
Your Study Strategy: A Proven 3-Phase Approach
Preparation for this exam demands structure, not randomness. Here’s a battle-tested 12-14 week plan.
Phase 1: Foundational Content Review (Weeks 1-6)
Goal: Build a comprehensive knowledge base across all 12 domains
Daily Tasks:
Dedicate each week to 1-2 domains
Read the relevant chapters in Bradley’s or Merritt’s
Take detailed notes focusing on clinical pearls, not every detail
Answer 30-50 topic-specific questions daily in “tutorial mode” (untimed, read every rationale)
Sample Weekly Schedule:
Week 1: Cerebrovascular disorders
Week 2: Epilepsy and seizures
Week 3: Headache and chronic pain
Week 4: Neuromuscular disorders
Week 5: Movement disorders + MS
Week 6: Infections, pediatric neurology, ethics
Time Commitment: 4-5 hours daily
Phase 2: Intensive MCQ Mastery (Weeks 7-12)
Goal: Become fluent in MCQ strategy and build exam-level endurance
Daily Tasks:
Complete 75-100 mixed MCQs in timed blocks (simulating exam conditions)
Set a timer for approximately 1.4 minutes per question (matching the real exam)
Review every single question—correct and incorrect
Maintain an error log noting which topics trip you up
Weekly Assessment:
Take a full-length mock exam (200 questions, 4 hours) on weekends
Track your score trajectory
If your score is below 65%, redouble focus on weak areas before moving forward
Time Commitment: 5-6 hours daily
Phase 3: Final Polish and Confidence Building (Weeks 13-14)
Goal: Fine-tune weak areas, build confidence, eliminate anxiety
Daily Tasks:
Focus exclusively on your weak topics (identified from mock exams)
Review high-yield facts and mnemonics
Take 2-3 more full-length mocks
Simulate exam-day conditions: early morning, no breaks, strict time limits
Exam Week:
Rest the day before; don’t cram new content
Review only your personal notes and error logs
Get adequate sleep; avoid exhaustion
Time Commitment: 4-5 hours daily
Essential Exam Strategy: How to Think Like a Test Taker
On exam day, your mindset matters as much as your knowledge.
The 1.4-Minute Rule
You have 240 minutes for 200 questions = 72 seconds per question. However, account for transitions and instructions. Aim to complete each question in 60-90 seconds maximum. This gives you a buffer for harder questions.
Read the Stem First, Then the Options
Don’t skim. Read the patient presentation carefully. Identify what the question is actually asking before looking at the options. Often, the last sentence of the stem is the actual question.
Use Elimination Aggressively
You don’t have to know the right answer—you just have to eliminate three wrong ones. In medicine:
Extreme answers (never, always) are often wrong
Answers that don’t match the clinical presentation can be eliminated immediately
Duplicate or very similar options suggest one is the correct answer
Flag and Move
If you can’t decide between two options within 90 seconds, flag the question and move on. Come back if time permits. Don’t waste time on one question while others remain untouched.
Answer Everything
There is NO negative marking. A blank answer is worth zero. A wild guess at least has a 25% chance of being correct (in a 4-option MCQ).
Trust Your Gut
If you studied well, your first instinct is often correct. Second-guessing yourself frequently leads to changing correct answers to incorrect ones.
Common Pitfalls and How to Avoid Them
Knowing what trips up other candidates can save you from the same mistakes.
Pitfall #1: Confusing Similar Seizure Types
Many candidates mix up absence seizures (3-Hz spike-and-wave, brief, no post-ictal confusion) with other generalized seizures. Memorize the EEG patterns and clinical features distinctly.
Pitfall #2: Over-Treating Hypertension in Acute Stroke
A common trap: candidates aggressively lower BP before thrombolysis when it’s actually unnecessary. Remember: BP < 185/110 is acceptable for thrombolysis. Don’t lower it unless specifically contraindicated.
Pitfall #3: Forgetting Patient Safety Questions
Candidates focus so much on disease knowledge that they miss straightforward patient safety, infection control, and ethics questions. These are “free points” if you’ve prepared.
Pitfall #4: Misjudging Question Difficulty
If a question seems too easy, it probably is. Don’t overthink simple questions. Conversely, if you don’t immediately know the answer, move on rather than dwelling.
Pitfall #5: Not Practicing Under Timed Conditions
Studying untimed questions is radically different from timed MCQs under pressure. Always practice with a timer running. Your performance will be 10-15% lower on timed questions compared to untimed practice.
Frequently Asked Questions
Q: Can I take the exam multiple times?
A: Yes, candidates typically get three attempts. If you fail three times, you may need professional retraining before a fourth attempt becomes available. However, most successful candidates pass on their first or second attempt with proper preparation.
Q: What if I trained in a non-English-speaking country?
A: The exam is in English. Make sure your English medical vocabulary is strong. Reading medical journals and listening to medical podcasts in English during your preparation phase helps.
Q: Should I memorize drug names or can I use generics during the exam?
A: The exam uses only generic drug names (e.g., metformin, atorvastatin, alteplase). You must be comfortable with generics, not brand names. During study, always use generic names.
Q: Is the exam different for consultant-level vs. specialist-level candidates?
A: The exam is the same. Only the passing score differs (70% for consultant vs. 65% for specialist). Study for 70% to ensure a comfortable pass at either level.
Q: How should I use online question banks?
A: Question banks are essential but should supplement, not replace, textbook reading. Use them primarily in Phases 2 and 3 when your foundation is already solid. In Phase 1, they should only reinforce what you’ve read.
Q: Can I get my exam fee refunded if I don’t pass?
A: No, exam fees are non-refundable, regardless of the outcome. However, you can reschedule within certain parameters if you need to postpone.
Q: What happens after I pass?
A: After passing, you’ll submit your exam result to SCFHS via Mumaris Plus. SCFHS will finalize your professional classification. From there, you’re eligible to apply for employment or licensure in Saudi Arabia and can apply to other GCC countries using your SCFHS classification.
The Takeaway: You Can Pass This Exam
The SCFHS Neurology Prometric exam is challenging, but it’s absolutely passable with disciplined, strategic preparation. The key differences between those who pass and those who fail aren’t intelligence or training background—they’re preparation strategy, consistency, and understanding what the exam actually tests.
You now have the official blueprint, the authentic content distribution, the recommended textbooks, and a proven study methodology. The rest depends on your commitment.
Start today. Follow the 3-phase plan. Use high-quality MCQ banks. Master the high-yield topics. On exam day, manage your time, trust your preparation, and answer every question.
Your neurologist’s license in the Gulf is waiting.
Have questions about your specific situation or need clarification on any exam requirement? Reach out—we’re here to help you succeed.