We have all experienced it: you wake up after sleeping on your arm, and your hand feels “asleep.” It buzzes, prickles, and feels heavy. A few shakes later, the sensation returns. This is normal.
But what happens when that feeling doesn’t go away? Or when it appears without a clear reason?
In medical terms, we call this sensation paresthesia. As a clinical neurophysiologist, I spend much of my time mapping the electrical signals of the nervous system to understand exactly where and why a patient is feeling numbness. If you are worried about persistent tingling, this guide will help you understand the potential causes and when to seek professional help.
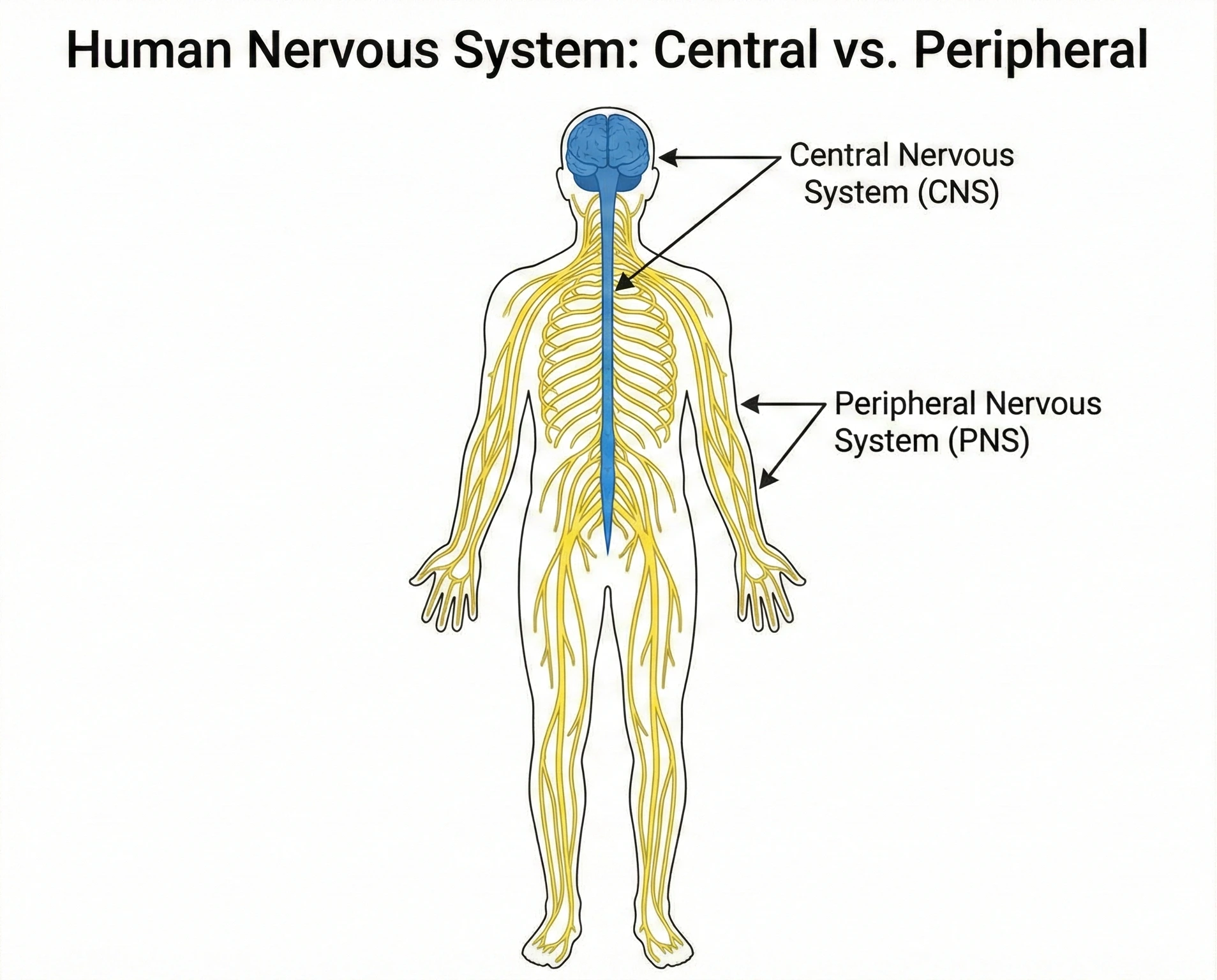
Understanding Your Nervous System: The “Wiring” of Your Body
To understand numbness, you have to picture your nervous system as a complex electrical grid.
The Brain and Spinal Cord are the “power plant.”
The Peripheral Nerves are the “wires” that travel out to your fingers and toes.
Numbness is simply a signal disruption. Somewhere along that line—whether at the spine, the elbow, or the wrist—the wire is being compressed or damaged, preventing the sensory signal from reaching your brain correctly.
Common Causes: Why Am I Numb?
In my clinic, the vast majority of numbness cases fall into three categories. Understanding the pattern of your numbness often points to the cause.
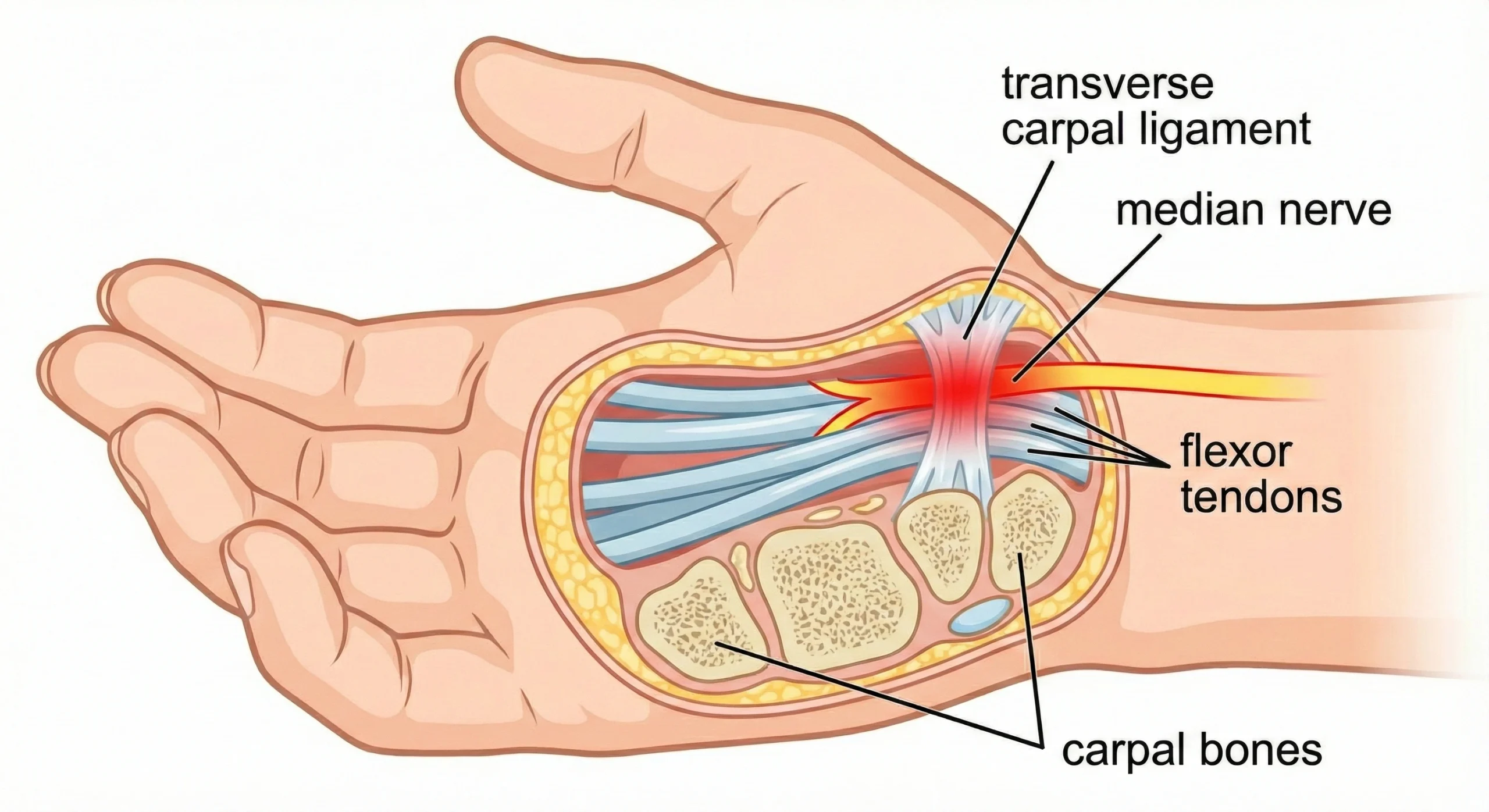
1. Entrapment Neuropathies (The “Pinched” Nerve)
This occurs when a peripheral nerve is compressed as it passes through a tight tunnel in your bones or muscles.
Carpal Tunnel Syndrome (Median Nerve): This is the most common cause of hand numbness. It typically affects the thumb, index, and middle fingers. Patients often tell me the pain is worse at night or when driving.
Cubital Tunnel Syndrome (Ulnar Nerve): If you lean on your elbows often, you may compress the ulnar nerve (“funny bone”). This causes numbness specifically in the ring and little fingers.
Meralgia Paresthetica: Compression of a nerve in the groin, causing burning or numbness on the outer thigh. This is common in pregnancy or with tight clothing.
2. Radiculopathy (The “Slipped Disc”)
If the problem isn’t in your hand or leg, it might be in your spine. When a disc herniates in your neck (cervical spine) or lower back (lumbar spine), it pinches the nerve root at the source.
The Key Sign: Radiculopathy rarely stays in one spot. It usually “shoots” or radiates down the arm or leg.
Dermatomes: We can often tell exactly which disc is injured just by where you feel the numbness. For example, numbness in the thumb often points to the C6 nerve root in the neck.
3. Peripheral Neuropathy (The “Dying Back” Phenomenon)
Unlike a pinched nerve (which affects one specific spot), peripheral neuropathy is a systemic issue affecting many nerves at once. It almost always follows a “stocking and glove” pattern:
It starts in the tips of the toes.
Over months or years, it creeps up to the knees.
Eventually, it affects the fingertips.
Common Culprits:
Diabetes: High blood sugar damages the tiny blood vessels feeding the nerves. This is the #1 cause of neuropathy worldwide.
Vitamin B12 Deficiency: Crucial for nerve health. A simple blood test can detect this.
Chemotherapy or Toxins: Certain medications can damage fragile nerve endings.
The “Red Flags”: When is Numbness an Emergency?
While most tingling is annoying rather than dangerous, there are specific patterns that require immediate medical attention. Go to the Emergency Room if:
Sudden Onset: The numbness hits you like a “thunderclap,” especially if it affects one entire side of your body (face, arm, and leg together). This is a classic sign of a Stroke.
Saddle Anesthesia: Numbness in your inner thighs, groin, or buttocks, especially if accompanied by incontinence (loss of bladder/bowel control). This suggests Cauda Equina Syndrome, a surgical emergency.
Rapid Ascending Weakness: Numbness starting in the feet and moving up to the legs within days, accompanied by weakness. This could be Guillain-Barré Syndrome.
How We Diagnose It: The Role of Neurophysiology
If you visit a neurologist, we don’t just guess; we test. The most valuable tool in our arsenal is the EMG/NCS (Electromyography and Nerve Conduction Study).
Many patients are anxious about this test, but it is the “gold standard” for diagnosis.
Nerve Conduction Study (NCS): We stick small patches to your skin and send tiny, safe electrical pulses to the nerve. We measure speed (how fast the wire is) and amplitude (how many fibers are alive).
Example: In Carpal Tunnel, the signal slows down drastically as it crosses the wrist.
Electromyography (EMG): We use a tiny, sterile pin to listen to the electrical activity of your muscles. This tells us if the nerve damage is permanent or healing.
Frequently Asked Questions (FAQ)
Q: Can anxiety cause numbness? A: Yes. During a panic attack, you may hyperventilate (breathe too fast). This changes the calcium levels in your blood, leading to tingling around the mouth and in the fingertips.
Q: Will the numbness go away on its own? A: It depends on the cause. “Saturday Night Palsy” (sleeping on your arm) usually resolves in weeks. However, numbness from diabetes or chronic compression (like Carpal Tunnel) often becomes permanent if not treated.
Q: Do I need an MRI? A: Not always. If your symptoms suggest a pinched nerve at the wrist or elbow, an EMG/NCS is actually more useful than an MRI. We usually reserve MRI for spinal or brain concerns.
Conclusion
Tingling and numbness are your body’s “Check Engine” light. It is a signal that a nerve is under stress. Whether it is a simple case of poor posture or a metabolic issue like diabetes, early diagnosis is key to preventing permanent damage.
If your symptoms are persistent, consult a neurologist or neurophysiologist. We can trace the signal to the source and help get your nerves firing correctly again.
Disclaimer: This article is for educational purposes only and does not constitute medical advice. If you are experiencing sudden or severe symptoms, please visit your nearest emergency department.